Capitol Coding Management Solutions
Maximize your CMS reimbursement revenue through accurate HCC coding.
Capitol Coding Management’s Restrospective / Prospective Risk Adjustment solution connects members with their physicians to proactively improve quality of care and risk score accuracy and identify actionable gaps in care, documentation, quality, assessment, and risk score accuracy. Interventions are implemented systematically and strategically, focusing on diagnoses that will have the greatest impact on reimbursement and member care.
We deliver significant financial value and improved care by coordinating the most appropriate interventions for identified members throughout the year.
Commercial risk adjustment is part of the Affordable Care Act. Its goal is to stabilize risk for individual and small group plans inside and outside of the Exchange marketplace. It helps health plans continue to offer much-needed coverage for a diverse population. With the Affordable Care Act’s risk adjustment mandate and the recent transition to ICD-10, there is increased focus on documentation and coding standards. Capitol coding Managements resources can help you improve documentation and coding.
- Chart Collection – Capitol Coding Management offers the provider HIPAA compliance and flexibility on how we collect the medical records. We provide the following options: onsite retrieval, submission by fax or email, EMR and EMR CCD data exchange.
- Data Validation – There is value in the compliance-based approach to this chart review. Our coding staff reviews the accuracy of existing diagnosis data from the health plan and provider. We can customize data to conduct multiple types of audits.
- Internal Mock RADV – This audit can assist the client on reducing their financial risk and alerting the health plans of codes that should be submitted to CMS for deletion. This process provides additional improvement for future audits and provider education.
- ACA HHS RADV – Our qualified coding staff performs risk adjustment data validation in accordance with HHS Inter-Rater Reliability requirements for the RADV. Capitol’s coding staff is trained and certified to review inpatient, outpatient, and professional settings.
Our mock audit process follows the CMS’ RADV audit model. Capitol Coding Management’s Mock RADV is designed to expose the full spectrum of strengths and weaknesses of a client’s readiness for RADV, both from a logistical and results perspective. Our team will identify specific medical records based on the high risk/high dollar factor, and review physician and coding documentation to confirm reported diagnoses and identifying coding errors.
This mock audit helps streamline your internal processes for an authentic RADV audit and helps to confirm reported diagnoses and identify ICD-10-CM coding errors. Errors in provider documentation are identified to prevent a negative impact on your overall RAF (Risk Adjustment Factor) score. Identifying missed diagnosis and accurately reporting those additional HCCs in RAPS filings typically result in millions of dollars of incremental revenue.
Capitol Coding Management manage healthcare outcomes and aim to enhance quality of care and reduce costs by meeting the performance measures.
Capitol Coding Management has nurses who specialize in HEDIS medical record review. We review the medical records provided by the client to find documentation for the annual HEDIS audit of care provided to Medicare members. The nursing staff reviews the data elements such as laboratory results, blood pressure, body mass index, colon cancer screening, and other aspects of care.
The medical record review on the members selected by the client will be performed according to the NCQA HEDIS specifications. Data will be entered using CCM Data Pro. The medical record will be reviewed for confirmation of member identification, data elements, numerator events and contraindications per HEDIS specifications.
Our nursing staff are experienced in acute care, primary care clinic, or disease management. They can remotely review the medical record through the client’s electronic medical record or by PDF paper chart provided by the client. The Capitol Coding Management staff complies with all applicable federal, state laws and regulations regarding health plan member privacy and data security, including HIPAA, the Standards for Privacy of Individually Identifiable Health Information, and the HIPAA Security Rule as outlined in the Code of Federal Regulations Title 45.
We understand that it is crucial to identify key data elements for reporting to acquire accreditation through NCQA. Here at Capitol Coding, we deliver a HEDIS Review process that is efficient and at the highest of quality to ensure the validity of the results.
Due to the consistent changes with the technical specifications, below are a few key elements that we ensure within our processes
- Annual HEDIS training to our Chart Specialist/Abstractors for specification changes
- Our Chart Specialist/Abstractors are trained for every project
- We conduct an over-read process to provide a secondary review on medical charts to maintain a 95% abstraction accuracy.
Capitol Coding Management Enhance compliance and identify undercoding, underreporting, overcoding, revenue opportunities, and avenues for documentation improvement.
Capitol Coding Management provides informative reports that reduces the client’s compliance risk. Our certified coders analyze complex code assignment options to select the appropriate code. The appropriate E/M code is assigned based on documentation in the medical record. We identify opportunities for increased revenue and ways to reduce compliance risks.We follow guidelines for facility E/M services and interpret the rules that govern E/M services for residents and fellows. The rules and regulations by Medicare are applied to the E/M services billed.
Evaluation and Management audits are available for all provider types. The following reports are provided:
- Provider audit summary report
- Provider results spreadsheet
- Provider scoring matrix based on percentages
- Provider scoring matrix based on point system
- 1995 & 1997 E/M documentation guidelines
A yearly sample E/M audit is recommended for each provider of a large practice. Quarterly evaluations are based on the provider’s percentage scoring matrix. Comprehensive results are outlined in the provider audit summary report. The patient medical record detail is provided with the provider result spreadsheet. The provider scoring matrix uses a point system to count the amount of errors on each section of the medical record.
Capitol Coding Management Train and assist providers to efficiently evaluate, document, code, and submit encounters based on the rules and regulations by all health plans.
The Capitol Coding Management’s provider outreach team provides extensive coding and documentation education to providers and office staff. All coders on staff are credentialed through the American Association of Professional Coders (AAPC) or the American Health Information Management Association (AHIMA). The coders are qualified to assign correct codes for CPT, HCPCS, ICD-10-CM, and ICD-10-PCS.
Our provider outreach training is designed to assist healthcare professionals to identify correct codes with their actual patient medical record. We provide current coding guidelines and appropriate documentation requirements based on the Centers for Medicare and Medicaid Services (CMS).
The following services are currently available and customized according to the client’s needs.
- HCC chart reviews Part C and Part D.
- HCC and Quality Measures for Annual Well Visit Form.
- Code capture from missed HCC opportunities based on claims data.
- Mock RADV for Commercial and Medicare Advantage.
- RADV for Commercial and Medicare Advantage.
- Evaluation and Management audit services.
- Create and revise medical practice superbills.
- Code assignment forall fee-for-service medical billing submissions.
- Practice medical management consultation.
Detailed reports with results and recommendations are presented to the client. Coding educational presentations are provided onsite or by webinar. We also assist with the client’s existing provider outreach team on the overflow of in-house projects.
We provide Best Practice Outsourcing Services for Document Retrieval and Scanning, empowering your organizational processes by converting documents into digital assets. Our services facilitate instant and secure access to information, enabling increased productivity, performance and profits.
We take every measure to ensure consistency and quality while minimizing variation by continually improving our processes. Our expert team serves as Outsourcing Partners and Solution Providers to companies that have critical document retrieval, scanning and imaging projects. Our Management Team has over 100 years of combined experience successfully designing and implementing document solutions.
The key to a successful project is starting with the end deliverable in mind, then employing proven technology solutions and conversion methods (of which scanning can be just one stage in the entire process). Successful document management requires a clear understanding of an organization’s Document Strategy, its People, Process, and Technology Requirements, and the optimal Implementation Approach.
We offer a unique blended centralized and onsite chart collection process that is tailored to your requirements. Whether records are scanned by providers and sent electronically to a centralized location or we dispatch a team of expert chart specialist onsite to a provider’s office to collect all required charts. Either options offer complete detailed chart collection to capture diagnoses and treatments for the most accurate HCC coding for retrospective / prospective risk adjustment and compliance with HEDIS and RADV requirements.
We can handle the details of a full range of requirements, including:
- Provider verification, including signature and specialty credentials
- Provider address and contact information
- Patient’s name and identity
- Dates of treatment or services
- Medical record fee reimbursement management
- Image quality and indexing specifications
We offer you consistent, efficient, affordable chart-retrieval services designed to achieve accurate appropriate CMS reimbursement.
Inpatient Coding Service
We specialize in providing contract, temp-to-perm, per diem, and direct hire personnel to practically every segment of the healthcare market.
Our medical coders can be deployed to work on-site or from a remote location. We assist providers in establishing both temporary and fully outsourced solutions. We are dedicated to delivering the most proven and competent medical coders at a moment’s notice. Whether our medical coders work on-site or off-site, their knowledge and training is second to none; they know the latest changes in coding regulations and the specialized coding needed for the newest clinical services. They have vast experience with coding thousands of patient records and are experts in all types of inpatient, outpatient and professional fee coding. We offer both coding and auditing services for inpatient records, Medicare and non-Medicare. Each coder/auditor whom we present to a client must undergo a thorough background check and proof of skills testing. The candidates’ skills are evaluated against tests that are developed in conjunction with the client.
Inpatient coding requires sound understanding of a broad range of complex diagnoses, procedures, and lab results. Coders who are proficient in this area have generally had several years of experience performing medical coding in an acute care hospital setting. The strong knowledge of anatomy and body system processes that comes with years of professional experience will be of critical importance for ICD-10-PCS.
The coding requirements for inpatient encounters contain many compliance challenges. Our coders become intimately familiar with your physician query procedures in order to provide documentation feedback in order to assist the client in full revenue capture.
Outpatient Coding Service
Our certified medical coders can be deployed onsite to the facility or off-site through remote access to the facility. Hospitals should consider performing coding reviews prior to billing, if practical. This kind of continuous, real-time auditing can identify patterns of problems with documentation or poor coding immediately. Otherwise quarterly or annual reviews should be performed on a retrospective basis.
Outpatient surgery coding, also known as same day surgeries, requires a very thorough knowledge of anatomy to appropriately assign CPT codes. Our coders ensure all procedures have a corresponding diagnosis that adheres to medically necessary payer and provider guidelines. Appropriate assignment of modifiers should also be reviewed as it affects APC assignment and thus reimbursement. APCs should be reviewed to validate appropriate transmission of HCPCS codes to the claim form. If the record shows that services were provided but not charged, then the department responsible should receive training or processes be revised. Our professionals understand the intricacies of global surgery package rules so that providers can stay in compliance with this very complex set of guidelines
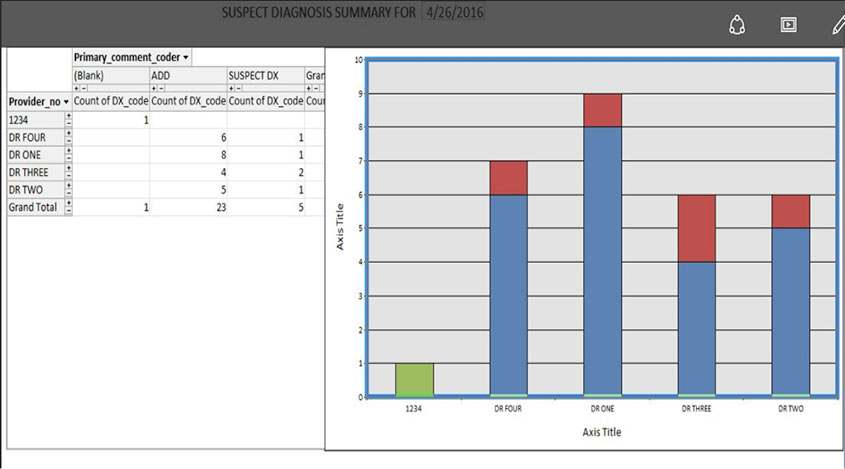
We have created a unique and customizable platform that adheres to our client specific needs. By integrating various tabs, mappings, reports and submission formats, we are able to implement functions for different scopes of projects.